During the changeover from RUG-IV to the Patient Driven Payment System (PDPM), all current Medicare A residents who were admitted prior to October 1, 2019 must receive an Interim Payment Assessment (IPA) under the PDPM, even if they were already assessed under RUG-IV. This is required in order to obtain a Health Insurance Prospective Payment System (HIPPS) code for billing purposes.
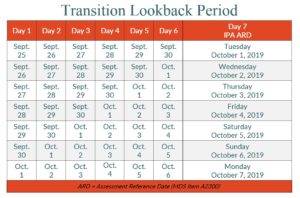
The Assessment Reference Date (ARD) for this transitional IPA must be set between October 1 and October 7.
As the last day of the look-back period, the ARD serves as the reference point for determining the care and services captured on the MDS assessment. Anything that happens after the ARD will not be captured on that MDS.
For example, for an MDS item with a 7-day look-back period, assessment information is collected for a 7-day period ending on and including the ARD which is the 7th day of this look-back period.
The look-back period includes observations and events through the end of the day (midnight) of the ARD.
As the transition period approaches, it may be helpful to give consideration to the optimal ARD for your transitional IPA assessments.
Click HERE to download a copy of this posting
This post is based upon details currently available from CMS at the time of publication. Please refer to the CMS PDPM page for more information.
